Developing Family Nursing
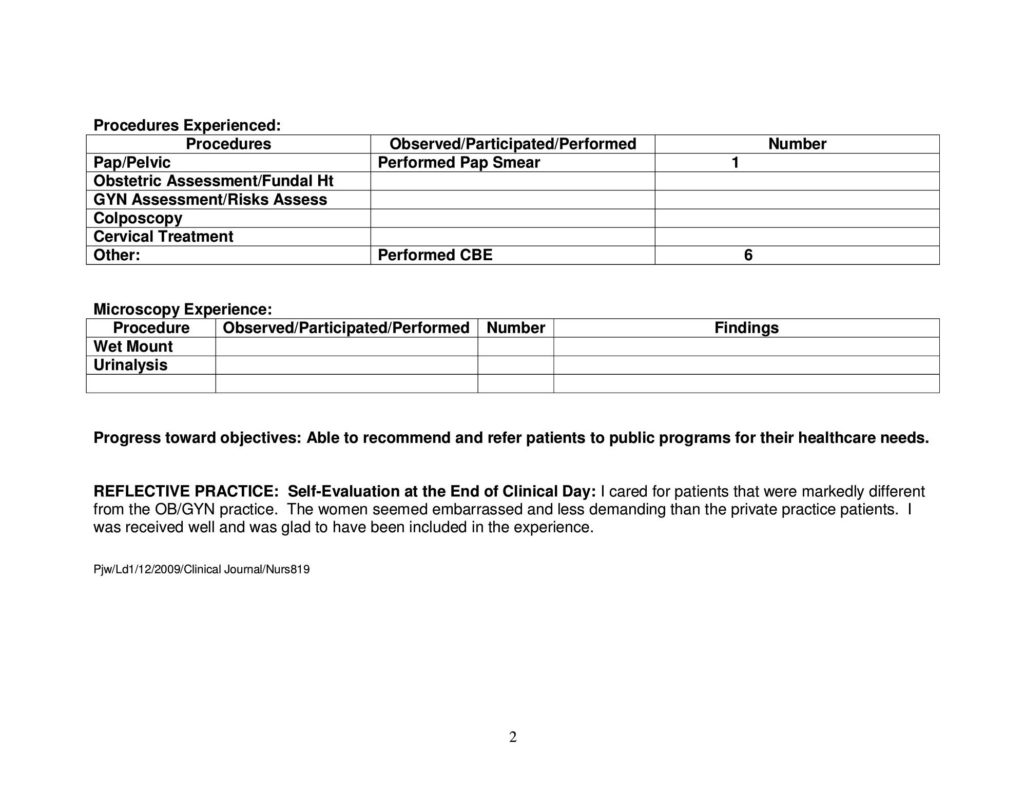
The didactic portion of the course provided instruction on theories and concepts related to nursing management in the care of developing families; critical thinking applied to health problems and needs of developing families, before, during and immediately following pregnancy; application of related nursing issues and current research. The clinical component allowed experiences and practice with developing families in a variety of settings. My clinical rotations included serving rural and underserved populations at the Sullivan Center and attendance in private practices in Clemson, SC and Greenville, SC.
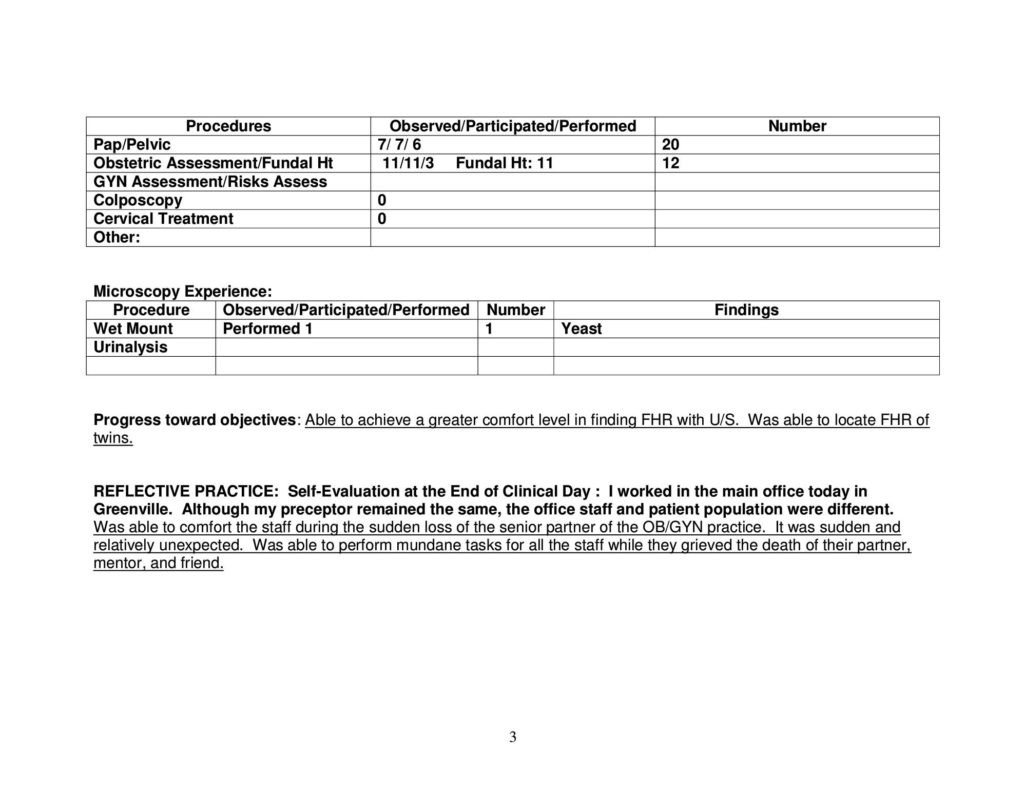
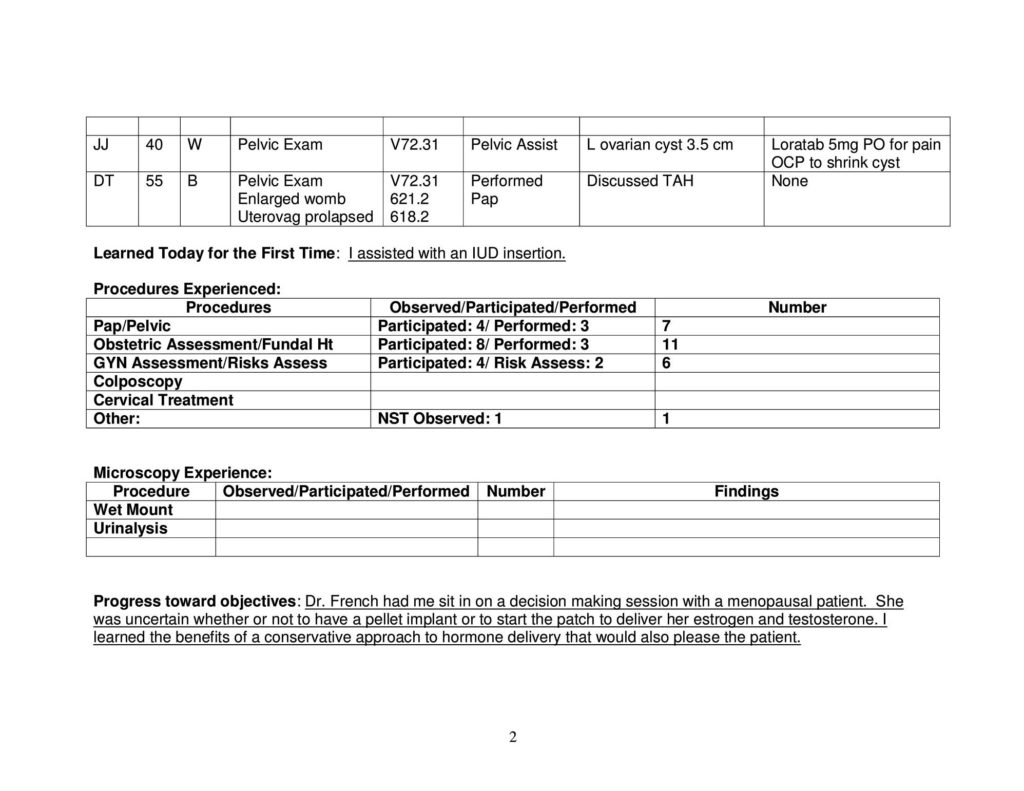
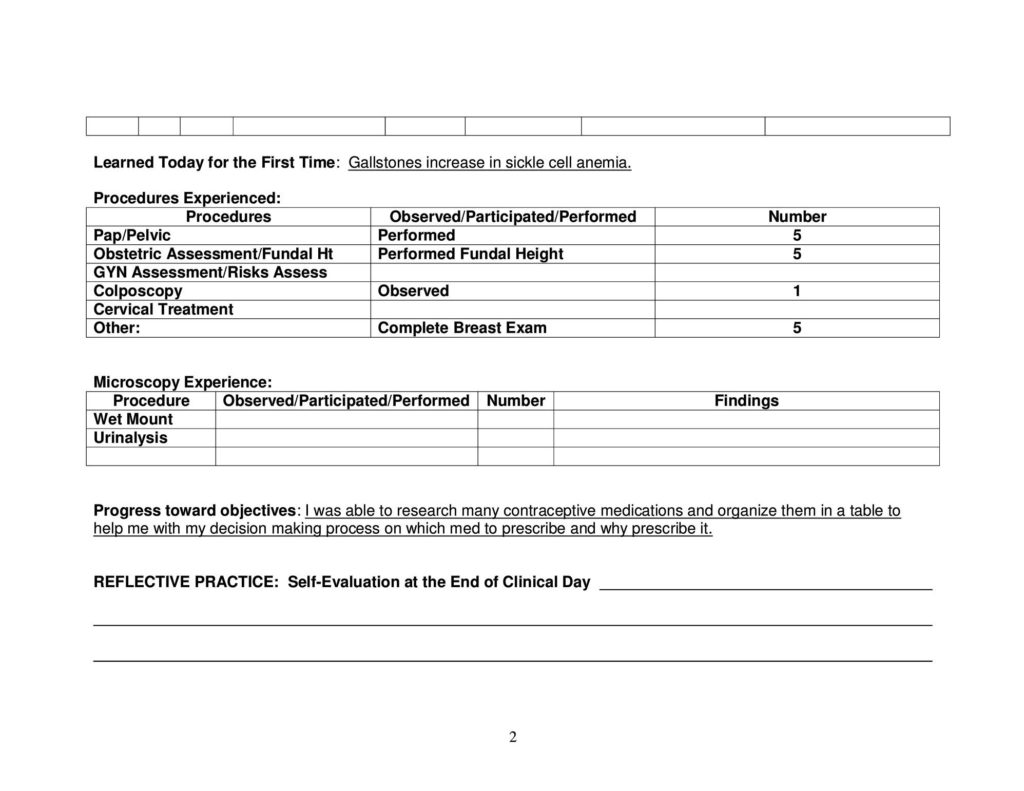
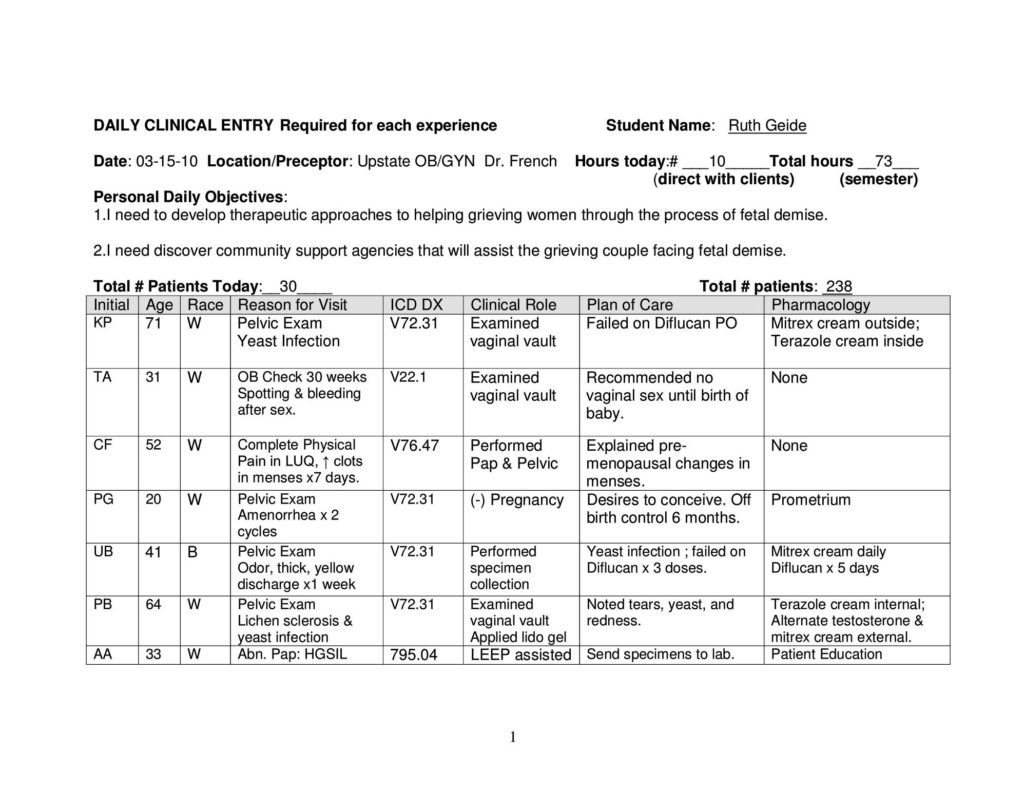
Total Patients: 300
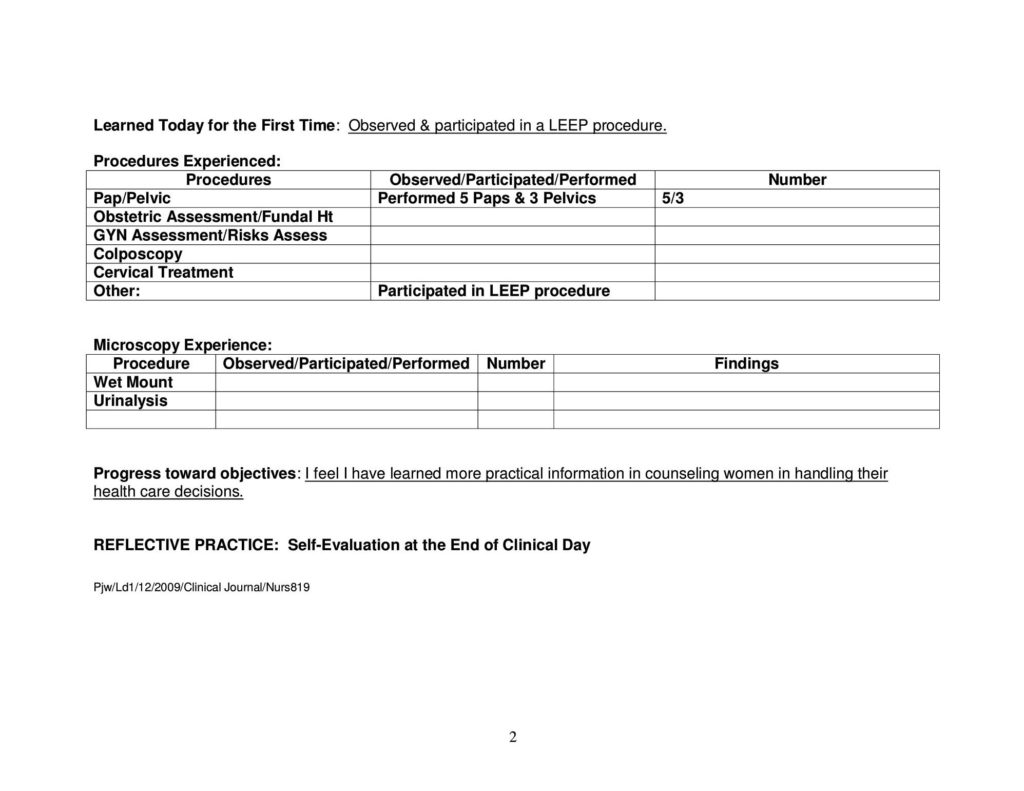
- 14 prenatal Visits & Fundal Exams
- 33 gynecology Visits (5 wet mounts, 2 pessary checks, 5 IUD removals)
- 5 Pap smears
- 19 pelvic exams
- 7 complete breast exams
Preceptors:
Dr. Paula Watt, PhD Sullivan Center
Dr. Martin French, MD Upstate OB/GYN
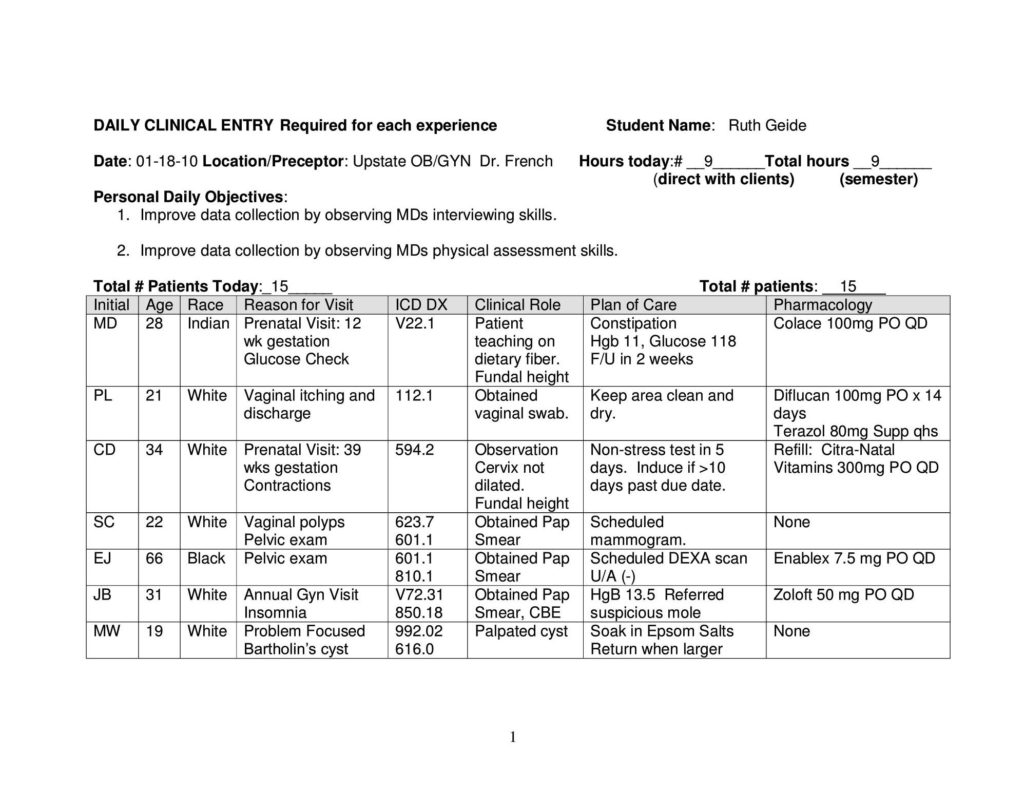
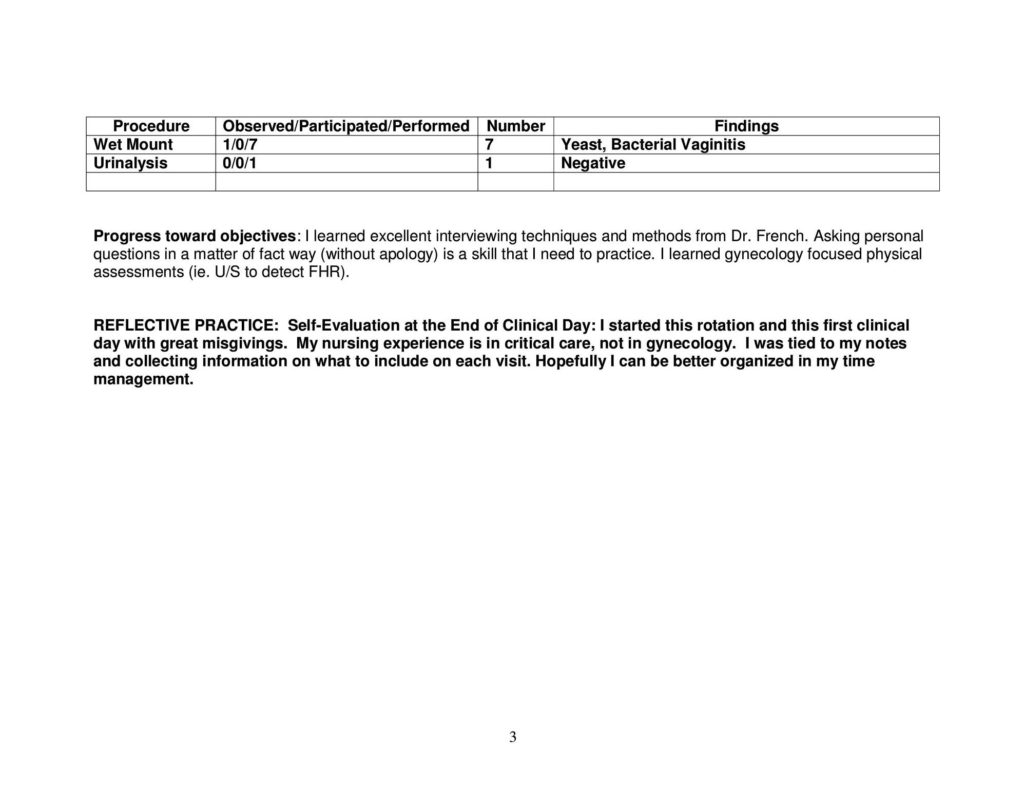
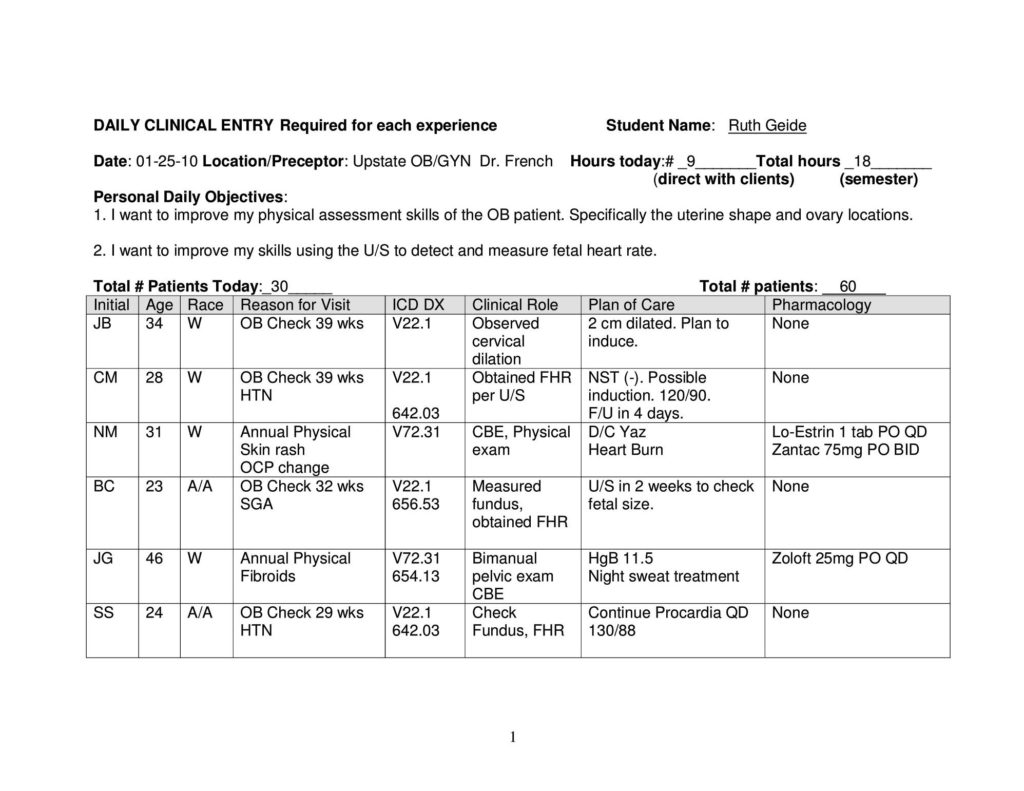
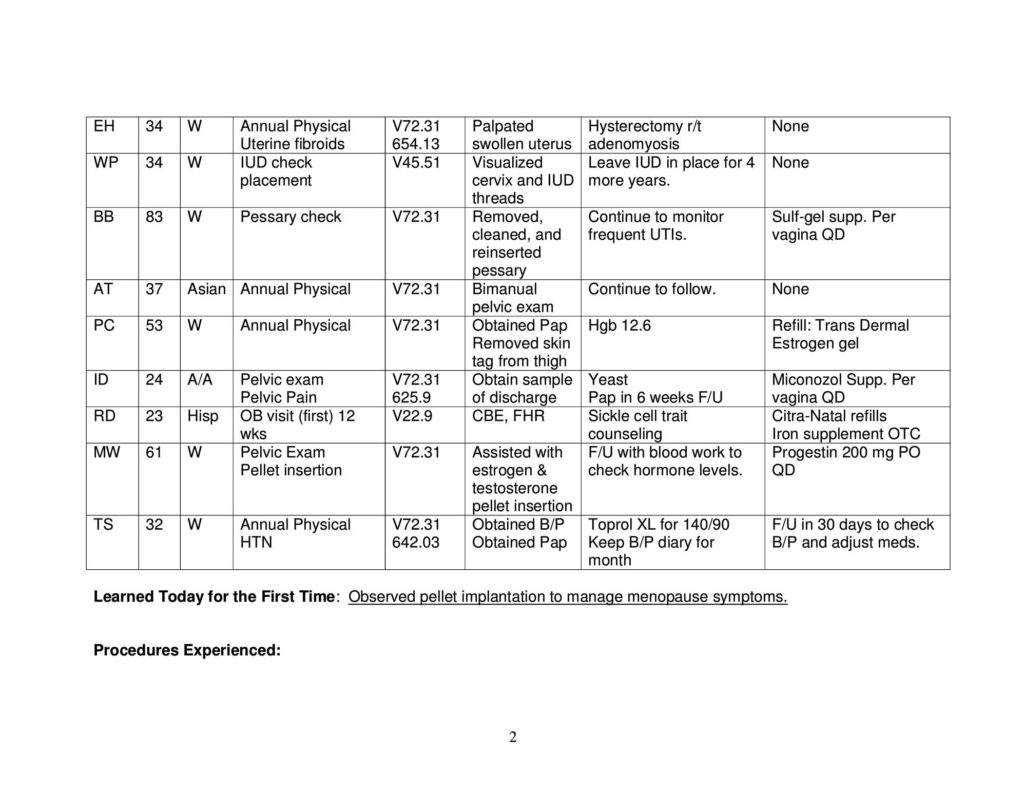
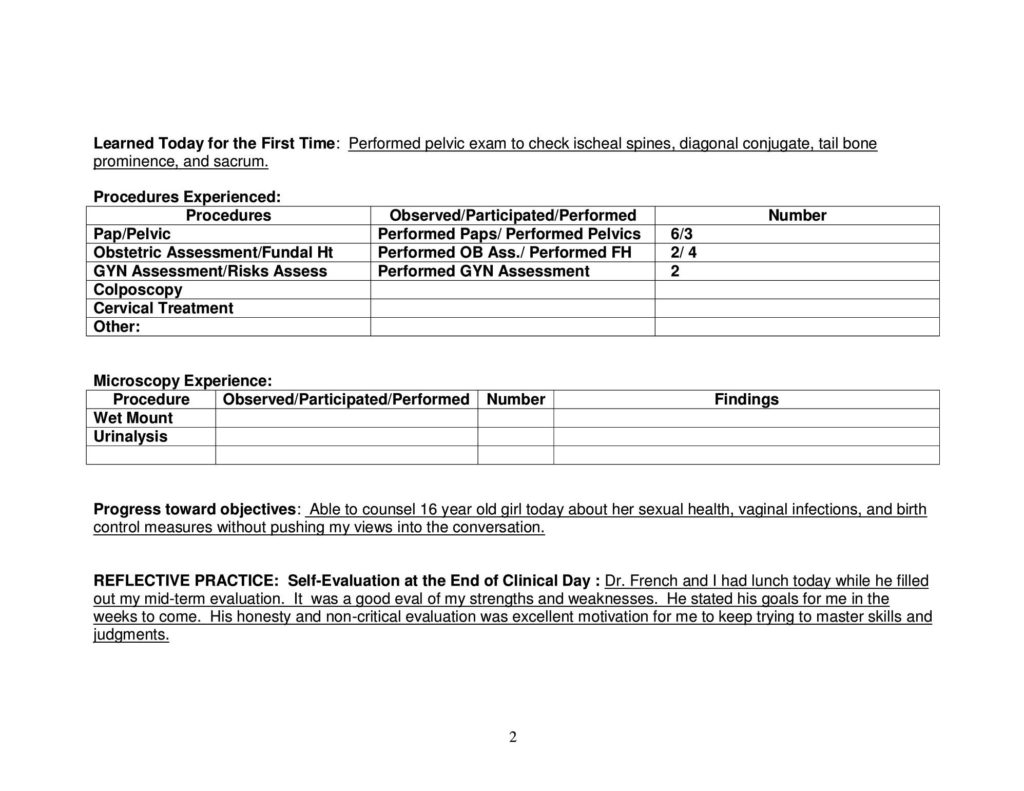
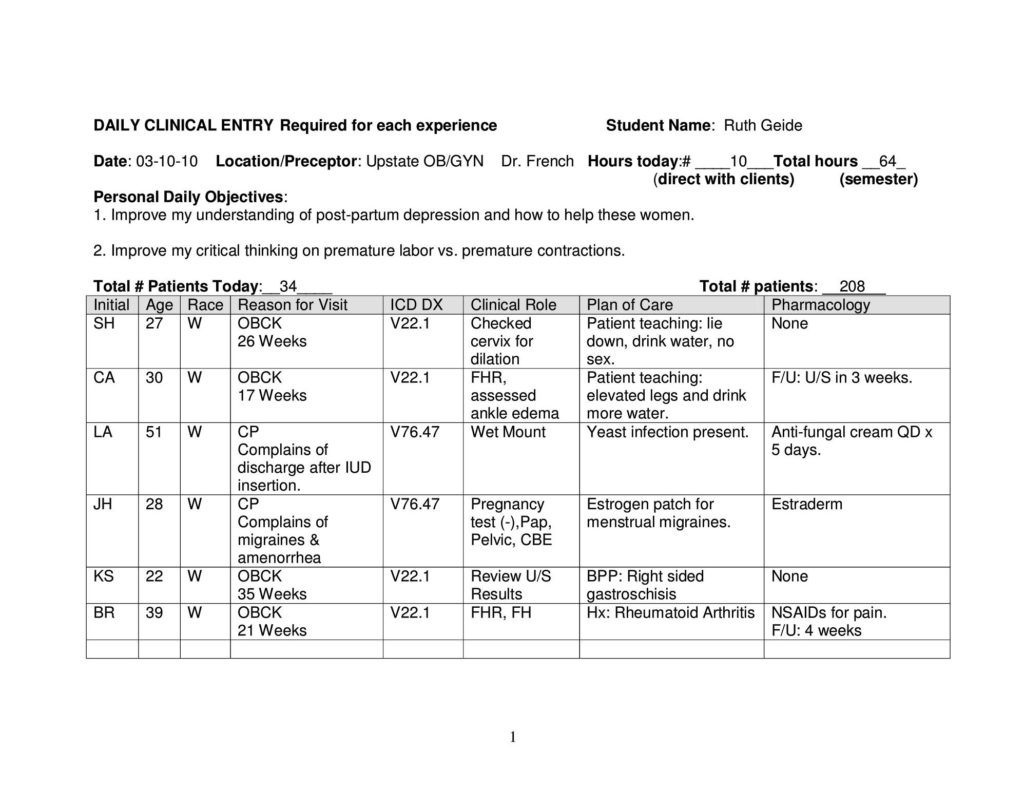
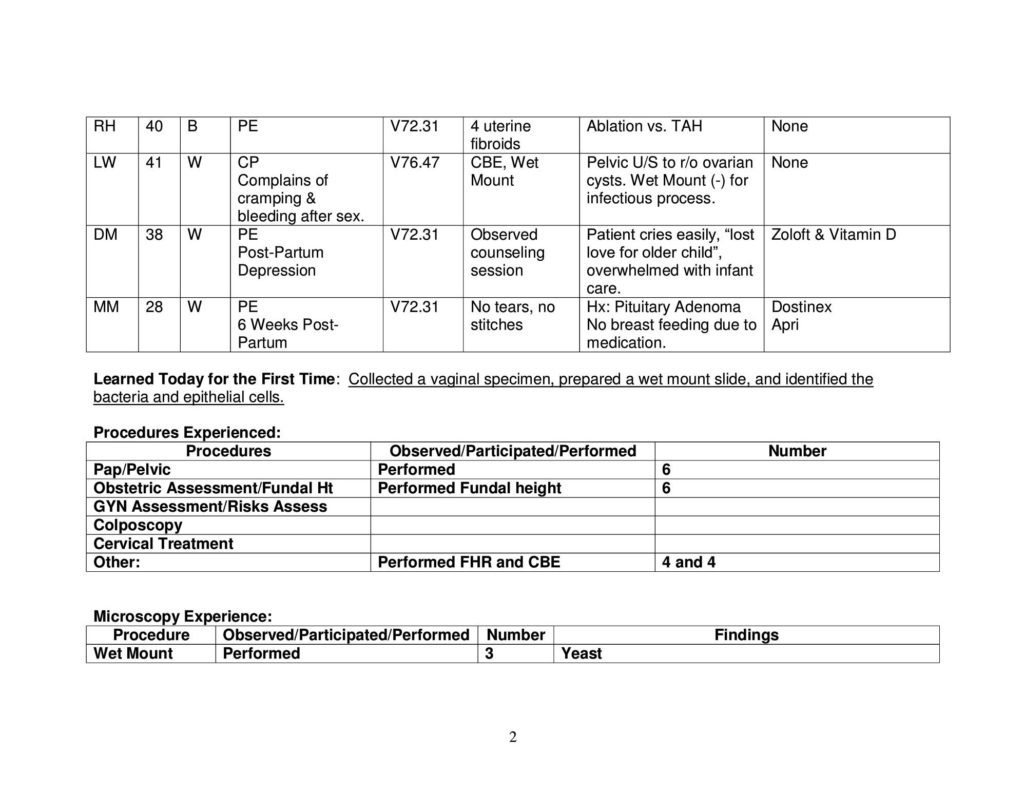
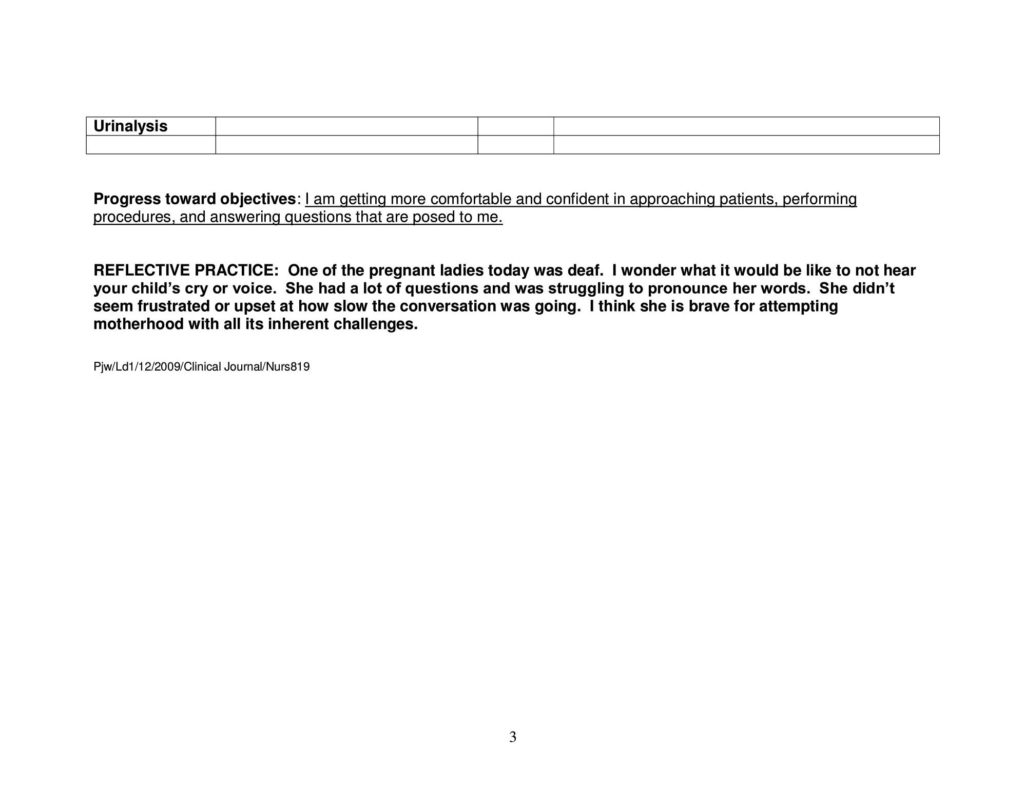
Developing Family Daily Patient Logs:











Preceptor Evaluation:


Course Project:
WOMEN’S HEALTH CASE STUDY
Ruth Geide
01-18-2010
HISTORY:
Current Complaint: EM is a 19 year old A/A female that presents today for a pre-college physical exam. She is also concerned about a recurrent pain in her LLQ and sacral area.
History of Present Illness: “I keep getting this bad pain low in my stomach and in my lower back every month just before my period starts.” She reports the “deep pain” to be a 6-7/10 that lasts for several days before the start of menses each month. She reports the pain to be worse than her normal cramps. The pain started in November, recurred in December and January. She reports mild relief from NSAIDs. She has noticed no spotting between periods, no change in her cycle length, or experienced any heavier menstrual flow over the past two months. She has not sought medical help with this cyclical pelvic pain because she “thought it would pass on its own”.
Past Medical History: She has had bronchitis and tonsillitis as a young child. Her immunizations are current as per the Anderson Health Department. She has no known allergies to food or medications. She is currently on no routine medications or daily supplements, only the NSAIDs as previously stated. She has had no hospitalizations, surgeries, or sports injuries.
Family History: Siblings as follows: One brother, age 22 in good health; one sister, age 16 in good health, and one sister deceased at age 14 due to MVA . Father diagnosed with HTN and DM II. Mother diagnosed with HTN and a history of endometriosis and TAH. Her paternal aunts and uncles have diagnosed HTN, CVD, and DM II. Her maternal aunts have diagnosed HTN, DM II, and breast cancer. Paternal grandparents are deceased, but had histories of stroke and breast cancer. Maternal grandmother is deceased due to suicide and had a history of breast cancer. Maternal grandfather has suffered a debilitative stroke. Please see genogram. She denies exposure to smoke.
Social History: EM is physically active in her high school sports program and enjoys a variety of friends. She denies smoking, alcohol, and prescription or illegal drug abuse. She is sexually active with her boyfriend, but can not be sure that he is exclusive with her. Her only contraceptive measure is withdrawal. She is looking forward to attending college in the Fall and majoring in economics.
Review of Systems:
General: Denies weakness, fevers, weight loss or gain.
Integument: Denies itching, rash, bruising, or lesions. Unaware of any bites or stings.
HEENT: Denies needing corrective lenses. Denies difficulty hearing. Annual dental exams.
Cardiac: Denies chest pain or palpitations.
Respiratory: Denies chronic cough, SOB, dyspnea, or wheezing. Denies hemoptysis.
Neurologic: Denies seizures, numbness, or tingling to extremities. Denies headaches.
GI: Denies difficulty swallowing, reflux or changes in appetite. Occasional constipation.
Psych: Denies episodes of depression, phobias, or suicide ideations.
Hematology: Denies history of bleeding tendency, excessive bruising, or sickle cell anemia.
Endocrine: Denies feeling jittery or fatigued due to thyroid dysfunction.
Musculoskeletal: Denies muscle aches or pains. Denies fractures due to falls.
GU: Denies frequency, urgency, or pain on urination.
GYN: Menarche began at age 11 with menses every 28 days lasting 5 days. Reports always having mild cramping during the first 2 days of menstruation. Reports pelvic and sacral pain occurring before menses as starting two months ago in November. LMP began 01-16-2010. Denies use of contraceptives. Denies ever being pregnant. Does not do monthly BSE. Denies any unusual vaginal discharge or itching.
Comprehensive Physical Exam:
General Survey: DOB: 06-29-1990; Vital signs: 98˚F; 64 reg.; 12 shallow & non-labored; 122/74 left arm; Height: 67 inches; Weight: 170 lbs. (77.27 kg); BMI: 26.6. EM is a well nourished, athletic -built and alert A/A female in no acute distress.
Integument: Warm, dry of flesh tone. No lesions, rashes, moles, or scars noted. No bruising or discolorations noted.
HEENT: Hair healthy, scalp free of lesions; Eyes clear, red reflex note, PERRLA. Vision 20/20 in both eyes. TMs clear, shiny, gray. Small amount of golden cerumen in external auditory canal. Hearing adequate at a conversational tone. Nasal mucosa pale pink, no drainage noted, septum intact. Denies sinus pain on palpation. Neck supple, no lymphadenopathy. Thyroid soft, normal size, no nodules noted on palpation. Pharynx pink and without exudate. Tonsils 1+. Oral mucosa pink, free of lesions, and well hydrated. Dentition intact, gums healthy. Tongue without lesions or furrows.
Cardiac: S1 & S2 without murmurs, gallops, or rubs. No carotid bruits noted. Peripheral pulses 2+.
Respiratory: Clear to all fields. No respiratory distress noted on deep breathing.
Neurologic: Cranial nerves I-XII grossly intact. Adequate sensation to pain in all extremities.
GI: (+) bowel sounds to all quadrants. Guarding to LLQ during palpation. No hepatosplenomegaly noted. Anal sphincter patent, no hemorrhoids noted. Stool specimen collected for occult blood. OB (-).
Psych: Affect appropriate, smiles and laughs frequently. Pleasantly cooperative during the examination.
Hematology: There were no previous labs for comparison. Fasting labs as follows for 01/18/2010:
CBC: RBC: 4.0; MCV: 90; MCH: 30; H/H: 14/45; BUN/Crt: 20/0.9; Glucose: 80
Chem-7: Na: 136; K+:4.5; Calcium:
Lipids: Triglycerides: 140; HDL: 100; LDL: 50; Total Chol: 150
Insulin:
Endocrine: Noted lipids on the high side of normal range and elevated insulin levels.
Musculoskeletal: Full ROM of all extremities, well coordinated movements
GU: Unable to palpate bladder. Noted urine to be clear and pale without sediment. U/A: Blood 2+, Ketones 1+, HgC (-)
GYN: Breast tissue firm; no masses or puckering noted; nipples symmetrical and not retracted. Patient on day three of menses. No unusual color or odor noted. Uterus tender to palpation. Tender nodular masses along uterosacral ligaments. External genitalia, cervix and vaginal mucosa are unremarkable. Pap Smear (-), Chlamydia (-), GC (-).
Risk Factor Assessment:
Medical/Family History/Race: Significant for DM, HTN, CVA, Breast Cancer, and Endrometriosis.
Heart Disease Risk Factor: 1% Risk of Heart Attack in 10 years.
IBIS Risk Factor: Risk after 10 years is 0.243%; Lifetime risk is 29.64%; Probability of BRCA 1 gene is 1.41%; Probability of BRCA 2 gene is 1.69%.
Medical/Personal: Sexually active (higher than average STDs & pregnancy), lipid levels, insulin levels. Interpretation
Management Plan: Consider both low income and insured.
Needs immunizations: Td boosters, meningococcal,HPV, H.Flu, Varicella
Test interpretations: Pap, GC, Chylamidia
Lab interpretations: BMI 26.6 (25-29.9=overweight, but waist <35”, >muscle mass)
OCPs to alleviate symptoms of endrometriosis & possible prophylaxis while waiting for laparoscopy for diagnostic confirmation.
Birth control counseling: consider what is easiest to use,store, and remember to take
Anticipatory Guidance: BSE, Erikson’s Stage: identity vs. role confusion; intimacy vs. isolation (psychosocial support from family & friends, involve parents & respected non-parent adults in developing problem solving skills through resiliency, need to develop and enhance a positive self-concept and self-esteem by recognizing & developing special skills & talents, Mental health (depression, anxiety, suicide) encourage to talk about underlying fears of separation from family,meeting new friends, & academic failures, dental: daily flossing & brushing, diet: unhealthy eating habits(180-230 grams of carbs daily, 0.8gm/kg/day of proteins, 5-9 servings of vegs & fruit), supplements(fish oil, iron, folic acid 0.4mg,Vitamin D 200IU, Calcium 1,000mg), safety :MVA + alcohol, rapes + dating violence (don’t overlook, forgive, or excuse the violence), increased personal freedom, lack of family and familiar support systems can increase risky behaviors; Piaget’s formal operational thinking=cognitive goal to think abstractly and logically; Kohlberg: separate from rules and expectations of parents and develop her own morality and define her personally held principles; identify & care for your spiritual needs
F/U: Needs yearly physical to track endo, DM, lipids, H/H, U/A, Influenza HTN, annual dental, annual eye exam, Pap annually until (-)x3, then q3 years
Will follow this patient and provide a medical home. Commend her for efforts and achievements. Schedule next visit, provide teaching pamphlets on birth control.
Course Project:
Clinical Protocol: Endometriosis (617.9)
Definition: Endometriosis is an estrogen-dependent inflammatory disorder in which cells lining the uterus (endometrium) implant in other locations in the body.
Etiology/Pathophysiology: The pathogenesis of endometriosis is unknown. In the 1920s, it was believed that endometriosis was caused by retrograde menstruation. Recent studies indicate the genetic allele HLA-B7 inhibits killer T and lymphocyte activity thereby allowing the ectopic sites to grow. Typically endometrial cells implant on the ovaries, fallopian tubes, bowel, rectum, bladder and the pelvic lining. Occasionally, some implants travel to distant organs such as the lung brain, and kidney. These ectopic implants grow and cause strictures and adhesions that obstruct the organ’s normal function. Advanced forms resemble blood-filled (chocolate) cysts and fibrotic lesions. Distortion of the fallopian tubes by these ectopic implants physically blocks the tubes and causes infertility.
Incidence/Demographics/Risk factors: Incidence: Found in 5-10% of women of reproductive age in the US. Endometriosis is the most common gynecologic reason for hospitalizations of females’ ages 15-44 years old. 25-35% of infertile women are diagnosed with endometriosis. 53% of adolescent females experiencing pelvic pain have endometriosis. The prevalence is also thought to be higher in white women and in those with lower BMIs.
Risk Factors: A woman with a first degree relative diagnosed with endometriosis is 6 times more likely to develop the condition. Early menarche, nuliparity, frequent menstrual cycles, menses lasting 7 days or more, and a closed hymen that blocks the menstrual flow are also common risk factors.
Classification/Staging: The staging of endometriosis does not classify the condition according to the severity of pain or other symptoms, but is meant to predict the chance of pregnancy. Points are arbitrarily assigned by the physician. Stage l: Minimal (1-5 points) isolated and superficial implants growing outside the uterus. Stage II: Mild (6-15 points) in addition to stage l findings there are also some deep lesions present in the cul-de-sac area. Stage III: Moderate (16-40 points) in addition to stage l & ll findings there are also implants found on the ovaries. Symptoms of endometriosis are common at this stage. Stage IV: Severe (>40 points) in addition to findings in stages l-lll there are large sized implants and extensive adhesions on several organs. Infertility is common at this stage.
Clinical: H&P/Labs/Differential Diagnoses/Signs and Symptoms:
History: Question client about pain: location (pelvic, sacral), onset (usually occurs a week or two before menstruation), duration (pain and cramps may be steady, dull, or severe and can be felt at any time during the menstrual cycle).
Signs and Symptoms: Some women may be asymptomatic even with severe cases. Pelvic pain and dyspareunia, bleeding with defecation, urination or intercourse may occur if the implants are on the rectum, urethra, cervix, vagina, or vulva. Inability to conceive if implants have occluded the fallopian tubes.
Physical findings: Pelvic exam reveals painful nodules in the posterior vaginal fornix, pain on uterine motion, fixed and retroverted uterus, and tender adnexal masses. Implants may also be found on healed episiotomy and cesarean section incisions or on the cervix.
Diagnostics: Ultrasound, x-ray, and CT scans are of little value. The CA-125 marker is an unreliable lab value as it can be elevated in other pelvic diseases. Final diagnosis can only be made by laparoscopy visualization. Implants on the ovaries appear as “chocolate cysts”, implants elsewhere can appear as red blotches of varying sizes, and some as dark spots resembling “powder burns”.
Differential Diagnosis: PID (614.9), pelvic /uterine adhesions (614.6), pregnancy (V22.2), leiomyoma (218.0), ovarian cancer (184.9), IBS (564.1), diverticulitis (562.11), ovarian cyst (620.0), adenomatous polyp (219.0), interstitial cystitis (595.1), uterine fibroids (621.8), dyspareunia (625.0).
Plan:
Monophasic OCPs for mild symptoms and for those not wishing to conceive. Prescribe for 6-12 months to decrease dysmenorrhea and to slow the progression of ectopic implants. Cost: $29.99/28 pack, Free at the health department, high co-pay with insurance. Progestins daily for 6-9 months to decrease growth of uterine lining. Provides partial or complete pain relief in 80% of women. Cost: $89.57/30 tabs; IM/q3mos/$94.58-191.59. High co-pay or not covered. A suppressive steroid with some androgenic properties that inhibits GnRH and ovarian release of estrogen (Danazol) bid 3-9 mos. Cost: $68.60-$110.76, low co pay. GnRH inhibitors for 6 months. This hormonal therapy inhibits ovarian release of estrogen and thereby inhibits the growth of the implants. Relieves moderate/severe pain. Cost: IM $355.97-$522.25/box, not covered by most insurance plans.
Other supportive: NSAIDs for mild pain as adjunct therapy. Cost: Wal-Mart $4, generics covered by insurance. SSRIs and SNRIs alleviate vasomotor symptoms. Cost: $80/30, high co pay or not covered. Relaxation techniques and acupuncture to help with pain management. There is insufficient evidence to recommend effective herbal products to manage symptoms at this time.
Follow up: Return to NP every 6-12 months to adjust or change medications due to complaints of side effects or to address compliance issues.
Refer/Consult: Moderate and severe cases will need to be referred to a surgeon for laparoscopic removal of implants. Laparoscopy does not cure endometriosis, but can provide pain relief when pharmacologic interventions have failed, cost: $1,700-$5,000. Total abdominal hysterectomy gives the best chance to cure endometriosis if the patient does not wish to conceive in the future, cost: $5,000.
Research: Prevention is not currently possible. More research and trials are needed before FDA approval can be granted for the following emerging therapies: antiprogestins, aromatase inhibitors, selective progesterone receptor modulators, and selective estrogen receptor-beta agonists.
Relevant References:
Bulun,S. (2009). Endometriosis mechanisms of disease. The New England Journal of Medicine, 360(3), 268-279.
Retrieved 01-18-10, from ProQuest Nursing & Allied Health Source, (Doc. ID: 1627865541).
DeCherney. A., Nathan, L., Goodwin, T., & Laufer, N. (2007). Current diagnosis & treatment obstetrics & gynecology
(10th ed.). New York: McGraw-Hill. 712-718.
Lee, S. (2009). Peritoneal Fluid Affects Release of IP-10 and IL-8 by Neutrophils & CD4 + T Cells. Fertility Weekly, 3-4
Retrieved 01-18-10 from Health source: Nursing/Academic Edition.
MyMedical Costs.com/Greenville, SC.
Nlm.nih.gov/medlineplus/ency/article/000915.htm
US Department of Health & Human Services Office on Women’s Health (2005, May). Endometriosis Guidelines.
Retrieved 01-22-10, from www.usdhhs.gov.
www.Online.Epocrites.com
N819/Spring 2010/RG
PowerPoint Presentation